Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here's a case that I saw of a 22 year old with Pedal Oedema and Shortness of Breath-
A young daily wage labourer presented with complaints of bilateral lower limb swelling from past 1 month, patient also had complaints of shortness of breath on exertion since 20 days which progressed to SOB at rest from the last 5 days.
For these complaints pt was taken to a nearby hospital and started on medication (no documentation) which he eventually stopped after 3 days claiming no health issue can happen to him. Patient had resumed his daily activities later on inspite of edema occurring intermittently. 8 days back patient was struck by grief after his grandfather expired and patient binged on alcohol the entire evening.
He developed pain abdomen the next morning which was maximum in intensity in the epigastric region. Patient also informs the nauseous feeling developed since then.
He complaints of reduced urine output in the past 4 days.
When he came to the hospital he had tachypnea and his bp was 80/50 mm hg for which we have started lasix but it kept dropping,so was started on nor adrenaline after which his blood pressure was stabilised.
Past History-
No similar complaints in the past.
Not a known case of Diabetes Mellitus, Hypertension, Asthma, Epilepsy, Tuberculosis, Cardiac or Thyroid Abnormalities.
Family History-
No similar complaints in the family.
Personal History-
Mixed diet.
Normal Appetite.
Adequate Sleep.
Regular Bowel and Bladder movements.
Addictions-
He is an alcoholic and is consuming toddy of about 1 litre,hooch of about 1 litre,180 ml of whisky on daily basis for the past 11 years.
General Examination-
Patient is conscious, coherent, cooperative.
Moderately built, Moderately nourished.
No pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
Bilateral Pedal Oedema Present (Pitting Type) till mid thigh.
Temperature- Afebrile
Blood Pressure- 80/50 mmHg(110/80 mm hg -morning 8 am)
Pulse Rate- 117 BPM(94)
Respiratory Rate- 30 CPM (26 )
GRBS- 221 mg/dl(116 mg/dl as of morning)
Systemic Examination-
Cardiovascular System-
Inspection-
Precordium apperars to be normal.
Skin over the chest is normal. No dilated vein, scars or sinuses.
Palpation-
Apex in the 6th ICS lateral to mid clavicular line
Parasternal heave present
JVP raised
Percussion-
Cardiac dullness till 6th ICS on left side.
Auscultation-
S1, S2 heard
No murmurs
Per Abdomen -
Inspection-
Shape of the Abdomen- Obese
Skin over the abdomen is normal.
All quadrants moving equally with respiration.
No visible pulsations, persistalisis.
No dilated veins. All hernial orifices are intact.
Palpation-
Diffuse tenderness all over the abdomen more in the epigastric region
No rebound tenderness. No guarding and rigidity. No organomegaly.
Percussion-
No dullness appreciated
Auscultation-
Bowel Sounds Heard.
Respiratory System-
Normal Vesicular Breath Sounds
No crepitations
Central Nervous System-
Cranial nerves-intact
Sensory system-stocking and glove pattern loss is seen
Motor system-
Tone-Normal
Reflexes-lost(all 4 limbs)
Power-5/5(all 4 limbs)
Treatment-
-soft diet
-Inj.Thiamine 1 amp in 100 ml NS
-Inj.Buscopan slow IV SOS
-Inj.Lasix 40 mg IV BD
-Inj.Pan 40 mg IV OD
-Tab.Ramipril 2.5 mg OD
-BP/PR/SPO2 and TEMP charting
-I/O charting
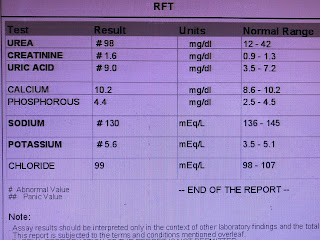
Investigations done-

24/09/2020 
25/09/2020






















Comments
Post a Comment